Senate report slams Medicare Advantage insurers for using predictive technology to deny claims
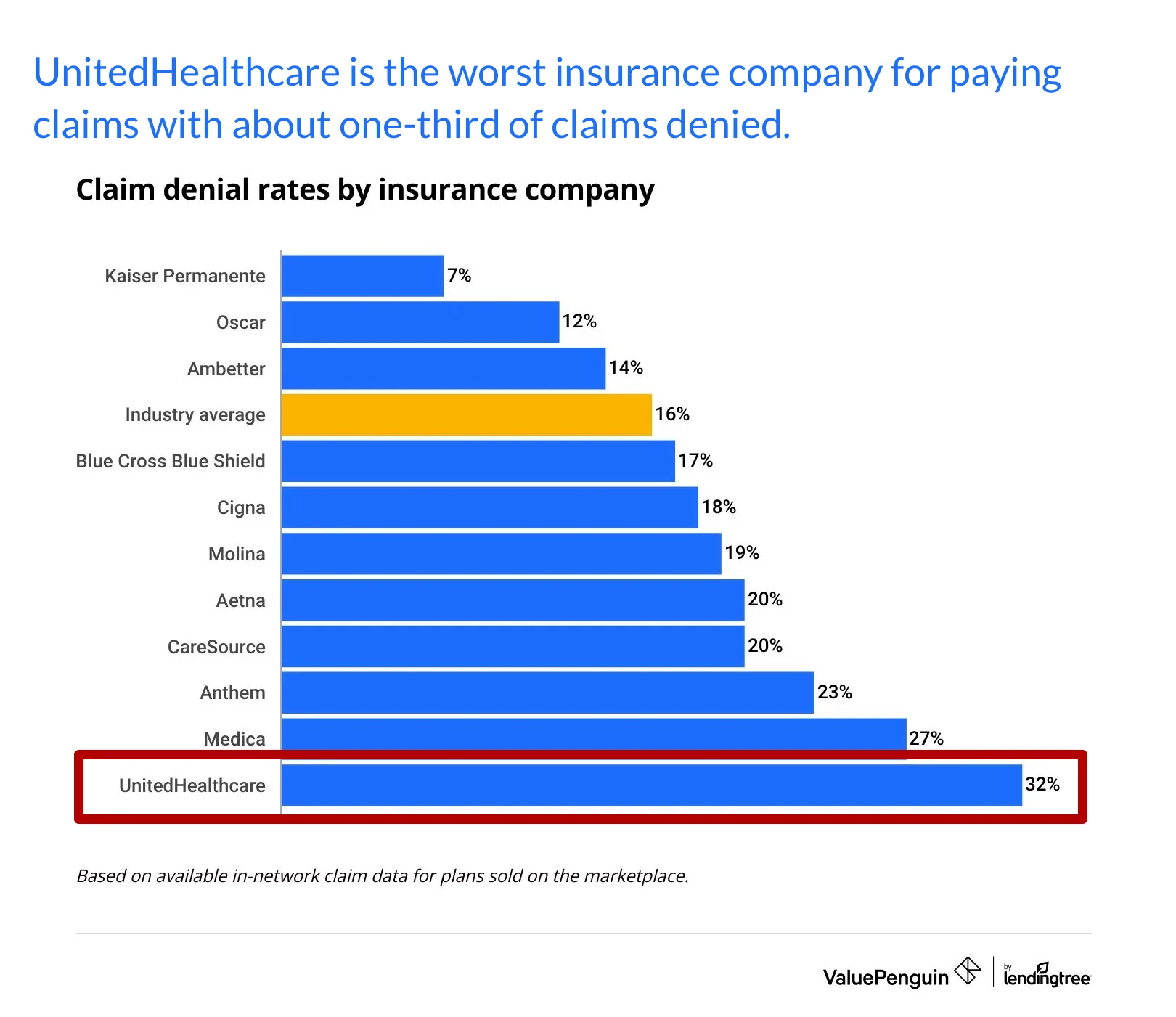
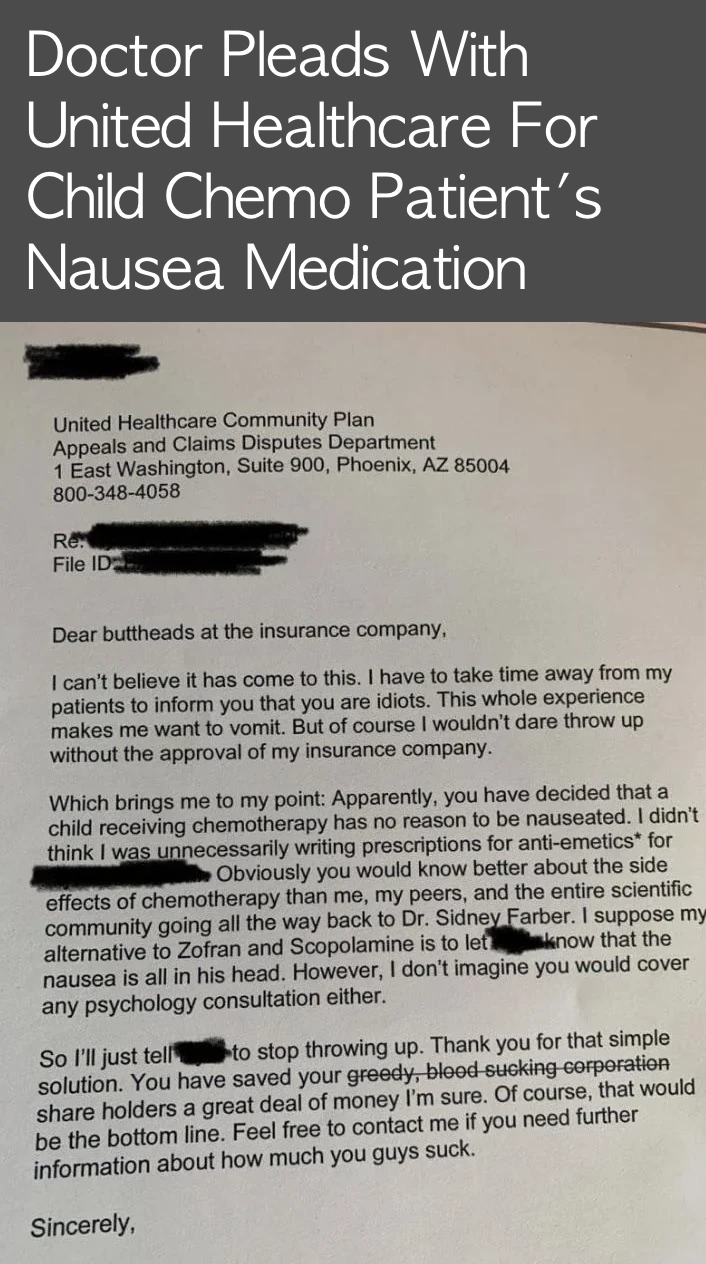
October 21, 2024. UnitedHealth, CVS and Humana used technology to increase MA prior authorization denials for post-acute services, boosting profits, according to a report for a Senate subcommittee. The insurers leveraged algorithmic tools to sharply increase claims denials for MA beneficiaries between 2019 and 2022, according to the report published Thursday by the Senate Permanent Subcommittee on Investigations. They most often denied coverage to patients in nursing homes, inpatient rehab hospitals and long-term hospitals, the report found.
UnitedHealth faces fines in California investigation
January 30, 2008. A California investigation into the claims practices of UnitedHealth Group has given fresh ammunition to opponents of UnitedHealth's buyout of local insurer Sierra Health Services, even as Sierra Health executives offered assurances that similar claims issues wouldn't happen here.
UnitedHealth could face fines up to $1.3 billion because its PacifiCare unit allegedly handled claims unfairly after UnitedHealth, the nation's second-largest health insurer, took it over.